Test Code:
902068
Clinical Use
-
Diagnose intestinal malabsorption and vitamin D deficiency or intoxication
- Monitor therapeutic response in patients being treated for vitamin D-related disorders
Clinical Background
25-Hydroxyvitamin D (25OHD) is the major circulating form of vitamin D and the precursor of the active form (1, 25-dihydroxyvitamin D). Because of its long half-life, 25OHD measurements are useful for assessing vitamin D status in patients.
Vitamin D occurs in 2 forms: vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol). Vitamin D3 is obtained from foods of animal origin and from ultraviolet light-stimulated conversion of 7-dehydrocholesterol in the skin, whereas small amounts of vitamin D2 are obtained from foods of plant origin. Both forms of the vitamin are used to fortify various foods and in over-the-counter supplements, and vitamin D2 is used in a high potency (50,000 IU) formulation for treating severe vitamin D deficiency. Furthermore, both forms are metabolized to their respective 25OHD forms (i.e., 25OHD3 and 25OHD2). Thus, analytical methods that can accurately quantitate both 25OHD forms are essential for diagnosis and monitoring patients with vitamin D disorders.
Most current methods do not differentiate between the 2 forms: only total 25OHD concentrations are reported. Additionally, some analytical methods may underestimate 25OHD concentration when significant amounts of 25OHD2 are present owing to diminished cross-reactivity.1 Other disadvantages to current methods include use of radioactive isotopes, method-to-method variation, and laboratory-to-laboratory variation.2 This liquid chromatography, tandem mass spectrometry (LC-MS/MS) method does not use radioisotopes and is sensitive and equally specific for both forms of 25OHD. Concentrations of each form are reported independently.
Individuals Suitable For Testing
- Individuals with suspected vitamin D deficiency (e.g., those with persistent, nonspecific musculoskeletal pain; the elderly; household individuals, etc.)
- Individuals with suspected toxicity (e.g., those with anemia of obscure origin, unexplained renal disease, etc.)3
- Individuals being treated for vitamin D-related disorders
- Individuals being treated for osteoporosis (More than 50% of women being treated for osteoporosis have vitamin D deficiency.)12
Specimen Requirements
0.3 mL room temperature, refrigerated, or frozen serum from a plain red-top tube or serum separator tube (0.15 mL minimum). Separate serum from cells immediately. Fasting preferred, but not required.
CPT Code*
82306
Method
Liquid chromatography, tandem mass spectrometry (LC-MS/MS)
- Extraction via protein precipitation
- Separation via high-performance liquid chromatography (HPLC)
- Detection and quantitation via tandem mass spectrometry
- 25OHD2 and 25OHD3 concentrations used to calculate total 25OHD levels
Reports include concentration of total 25OHD, 25OHD2, and 25OHD3
Analytical sensitivity: 4 ng/dL for 25OHD2 and 25OHD3
Analytical specificity: no cross-reaction with vitamin D2 or D3; 1α,25(OH)2D2; 1α,25(OH)2D3, calcitrol; 25,26(OH)2D3; 1α(OH)D2, doxercalciferol; and 1α(OH)D3, alfacalcidol
Reportable range: 4 – 512 ng/mL for 25OHD2 and 25OHD3
Aliases: 25OHD, 25-hydroxycholecalciferol, 25-hyrdoxyergocalciferol
Reference Range
The reference range for total 25OHD (20-100 ng/mL) is based on 25OHD correlation with physiological parameters that include parathyroid hormone concentrations and calcium absorption.4-8 The range is not based on the distribution of levels in an apparently healthy population. 25OHD2- and 25OHD3-specific reference ranges are not available.
Interpretive Information
Decreased 25OHD concentrations are an indication of vitamin D deficiency and are associated with hypocalcemia, hypophosphatemia, and elevated alkaline phosphatase. In addition to insufficient intake or production, disorders that are characterized by deceased absorption or excessive loss in the gastrointestinal tract, increased vitamin D metabolism, or impaired conversion of vitamin D to 25OHD can cause decreased 25OHD levels (Table).
Elevated levels of 25OHD suggest vitamin D intoxication and distinguish this disorder from other hypercalcemia-causing disorders.
Levels may vary with exposure to sunlight, peaking in the summer months.
Table. 25-Hydroxyvitamin D (25OHD) Concentration in Various Disorders9-11
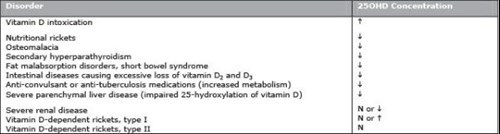
N = normal
References
- Hollis BW. Comparison of commercially available 125I-based RIA methods for the determination of circulating 25-hydroxyvitamin D. Clin Chem. 2000;46:1657-1661.
- Binkley N, Krueger D, Cowgill CS, et al. Assay variation confounds the diagnosis of hypovitaminosis D: a call for standardization. J Clin Endocrinol Metab. 2004;89:3152-3157.
- Koutkia P, Chen TC, Holick MF. Vitamin D intoxication associated with an over-the-counter supplement. N Engl J Med. 2001;345:66-67.
- Hollis BW. Circulating 25-hydroxyvitamin D levels indicative of vitamin D sufficiency: implications for establishing a new effective dietary intake recommendation for vitamin D. J Nutr. 2005;135:317-322.
- Holick MF. Vitamin D deficiency: what a pain it is. Mayo Clin Proc. 2003;78:1457-1459.
- Lips P, Duong T, Oleksik A, et al. A global study of vitamin D status and parathyroid function in postmenopausal women with osteoporosis: baseline data from the multiple outcomes of raloxifene evaluation clinical trial. J Clin Endocrinol Metab. 2001;86:1212-1221.
- Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet.1998;351:805-806.
- Plotnikoff GA, Quigley JM. Prevalence of severe hypovitaminosis D in patients with persistent, nonspecific musculoskeletal pain. Mayo Clin Proc. 2003;78:1463-1470.
- Bringhurst FR, Demay MB, Kronenberg HM. Hormones and disorders of mineral metabolism. In: Larsen PR, Kronenberg HM, Melmed S, Polonsky KS, eds. Williams Textbook of Endocrinology. 10th ed. Philadelphia, PA: WB Saunders; 2003:1303-1371.
- St-Arnuad R, Glorieux FH. Hereditary defects in vitamin D metabolism and action. In: DeGroot LJ, Jameson JL, et al, eds. Endocrinology. 4th ed. Philadelphia, PA: WB Saunders; 2001:1154-1168.
- Goldring SR, Krane SM, Avioli LV. Disorders of calcification: osteomalacia and rickets. In: DeGroot LJ, Jameson JL, et al, eds. Endocrinology. 4th ed. Philadelphia, PA: WB Saunders; 2001:1223-1243.
- Holick M, et al. Prevalence of Vitamin D Inadequacy Among Postmenopausal North American Women Receiving Osteoporosis Therapy. JCEM 90(6):3215-3224.
*The CPT codes provided are based on AMA guidelines and are for informational purposes only. CPT coding is the sole responsibility of the billing party. Please direct any questions regarding coding to the payor being billed.
